Claims Processing Automation.
Dealing with claims can be time-consuming, often taking up to 30 days to review each case due to the volume of required documents. When you have dozens or even hundreds of cases to handle daily, manual processing can be risky, as it is prone to human error, leading to delays and unhappy customers. It's also tough to spot fraudulent documents, which can result in compliance issues.
The good news is that there's a solution: DocHorizon, our intelligent document processing platform, automates data extraction, making your document-related tasks much easier, saving you time and resources.
Features of Automated Claims Processing.
Intuitive User Interface
Effortlessly automate your document workflows with our low-code platform. Tailor and streamline your claims processes to perfectly fit your business needs without requiring extensive coding knowledge. Our intuitive drag-and-drop functionality makes customisation a breeze.
Precision Data Extraction
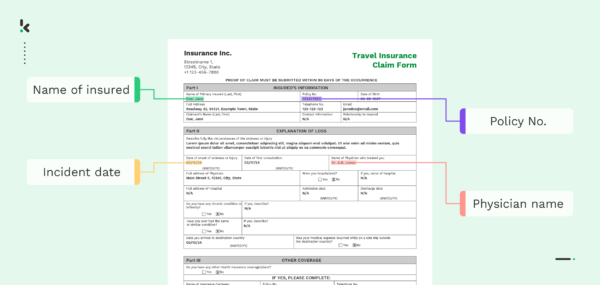
Our cutting-edge intelligent document processing solution incorporates advanced optical character recognition (OCR) software, meticulously extracting structured data with over 99% precision from any section of your claims documents, ensuring efficient and accurate data extraction.
Integrated Fraud Detection
Our platform is equipped with advanced technologies such as duplicate detection and EXIF analysis, enabling early identification of fraudulent documents and preventing attempts to bypass the system. This helps maintain the security and integrity of your claims processing workflow.
Seamless API Integration
Connect our document processing technology to your own applications via API for a streamlined workflow. We offer seamless integration features with existing business systems, practice management software, and databases for efficient and effective implementation.

Data Security & Compliance
Our solution includes robust security and compliance measures to prevent data breaches and unauthorised access. For example, our data masking feature ensures compliance with regulations like the Data Protection Act by obscuring sensitive data before transmission to databases.
We're Here to Help! Ask Us Anything.
Contact usBenefits of Automated Claims Processing.
Increased Efficiency & Accuracy
Automation reduces errors associated with manual claims processing and ensures consistency, improving efficiency and accuracy.
Cost Savings
Automation reduces labour costs associated with resource-intensive claims processes, leading to significant cost savings.
Better Customer Experience
Automation allows adjusters to focus on going the extra mile for policyholders instead of data entry, enhancing customer communication.
Minimised Errors
Our automated IDP solution eliminates manual data entry and verification errors, ensuring accurate and timely claims processing.
Simplified Compliance
Automation facilitates regulatory compliance, reducing the risk of fines and penalties caused by fatigue, negligence, or deception.
Fraud Prevention
Our automated IDP solution is adept at detecting document fraud, minimising the risk of unjustified payments for ineligible claims.
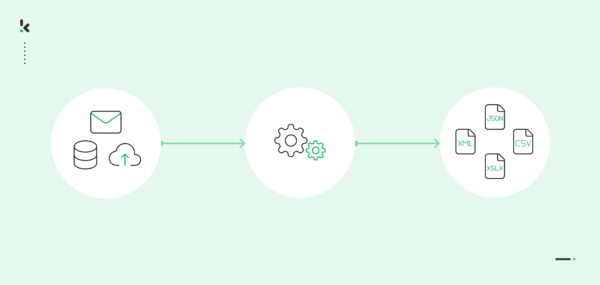
How It Works.
Filing a Claim
You can submit the FNOL directly to the platform via web application, FTP, or email. Alternatively, scan or photograph documents with our SDK and upload the digital images via API.
Claim Validation
Claim data is stored centrally, with all relevant documentation converted into machine text via OCR and compared to the customer's policy to assess the claim's validity.
Claim Verification
The system automatically collects repair cost estimates and other relevant third-party data, then compares it against external sources to assess potential fraud in the claim.
Claim Adjustment
AI algorithms suggest the appropriate payment amount based on the damage or costs incurred and the customer’s policy coverage. The policyholder decides whether to settle or negotiate.
Our Customers.
What Our Customers Say.
Our Accreditations.
Frequently Asked Questions.
What is claims processing automation?
Claims processing automation involves leveraging technology to automate the processing of documents for insurance claims. By using automation, claims examiners, clerks, and adjusters can extract data from documents and automatically verify it, leading to quicker decision-making. Claims processing entails verifying various documents to determine the claimant’s eligibility for compensation. Common documents involved in claims processing include:
- Invoices
- Receipts
- Insurance claim forms
- Proof of ownership or residency
- Identity documents
- Insurance cards
- Medical prescriptions
What are the main steps in claims processing?
The typical claims process consists of six steps from the initial report to the final decision. Each step may necessitate documentation to guarantee accuracy, compliance, and efficiency. The key steps in claims processing are as follows:
- Claim Reporting: The insured reports a claim by filling out an insurance claim form, providing details such as the date, time, location, and reason for compensation. Automation can expedite the case opening process, especially in health insurance claims by extracting key details.
- Claim Investigation: The claims team conducts a thorough investigation to authenticate the claim and requests relevant documentation or evidence. Automation can accelerate this process.
- Claim Assessment: After gathering information as per the insurance policy, the damage and settling costs are evaluated, considering any applicable deductibles. Automation can speed up this assessment process.
- Settlement Offer: Based on the assessment, a settlement offer is made to the policyholder, describing the compensation or assistance for the damage sustained.
- Negotiation (if necessary): If the insured disagrees with the offer, negotiations can take place to reach a resolution.
- Resolution and Closure: Upon reaching an agreement, the claim process is finished, and the agreed-upon compensation or assistance is provided. Any remaining disputes are addressed until a resolution is reached, and the claim file is closed.
Why automate claims processing?
In our experience, there are five common indicators that suggest an insurance company can benefit from automated claims processing:
- A surge in claims, particularly during natural disasters, causes significant slowdowns in processing, leading to customer dissatisfaction.
- Claims leakage, which represents the difference between actual and optimal payment due to processing inefficiencies, reaches as high as 20-30%.
- Customer satisfaction and net promoter scores are below expectations, and customer churn coincides with claim settlement times.
- Inability to obtain a comprehensive view of each claim and customer due to disorganised and unstandardised data.
- Data extraction, entry, and verification are ongoing tasks, leading to decreased productivity.
How does claims processing automation work?
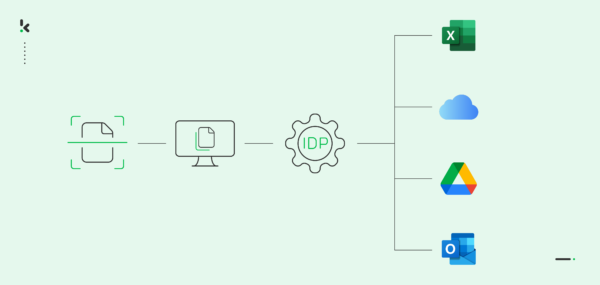
Intelligent document processing solutions, like DocHorizon, serve as the primary technology driving claims process automation. DocHorizon integrates multiple components, including Optical Character Recognition (OCR), to collaborate in automating the entire document workflow.
Here are some of the technologies at play, how they work, and how they can help you with claims processing automation.
- Artificial Intelligence (AI): AI can extract meaning from documents or handwritten texts, saving time and reducing errors, leading to efficient and accurate automated claims processing.
- Natural Language Processing (NLP): NLP helps computers understand natural language, enabling easier document categorisation within claims processing.
- Machine Learning (ML): ML improves data accuracy over time, enabling informed decision-making and aiding in the identification of suspicious activities indicative of fraudulent claims.
- Robotic Process Automation (RPA): RPA deploys software robots to handle tasks such as data extraction from documents, form filling, validation, communication with other systems, and fraud detection, streamlining the entire claims process.
These technologies enhance automation by reducing errors, improving efficiency, and freeing up human resources for more critical tasks within insurance claims processing.